Post-Concussion Care Pathway
There are a few caveats that must be noted right upfront:
- A large proportion of persons who sustain a concussion will experience resolution of symptoms within the first several weeks. This proportion would follow the green parts of the pathway diagram below. A smaller proportion (approximately 15 -20%) of individuals will go on to require interdisciplinary concussion clinic care and they would follow the yellow through to red parts of the pathway diagram below.
- Treatment and care should be consistent with best practice according to the Living Concussion Guidelines: Guideline for Concussion & Prolonged Symptoms for Adults 18 Years of Age or Older or the Guidelines for Diagnosing and Managing Pediatric Concussion.
- At multiple times after the incidence of the concussion it is essential that both written and verbal education be provided regarding recovery, treatment and symptoms. This is shown by the blue starbursts in the diagram below.
A pathway of post-concussion care was developed that would be applicable across the province to patients while accounting for the vast regional differences.
All suspected concussions should be assessed by a medical professional as per the pathway. This is to rule out the presence of other medical conditions and ensure that any symptoms that develop or worsen get the needed medical follow-up. If someone were to seek treatment from a health care provider without having been medically assessed, they should be directed to the top of the pathway.
In the minority of cases where symptoms are not resolving within 2 weeks, it is recommended that there be re-evaluation by a physician and additional diagnostic assessment(s). The diagnosis of concussion is a clinical diagnosis based on observed symptoms, mechanism of injury and clinical history. Symptoms after concussion can be physical, cognitive and social/emotional and all must be assessed to inform a concussion diagnosis. Physicians, nurse practitioners and neuropsychologists are able to diagnose concussion; however, it is important that a medical assessment be conducted first to ensure medical stability.
For patients requiring interdisciplinary care it is desirable to have providers who are treating the same patient located in the same clinic as this helps inter-professional communication and collaboration; however, this is not always possible. When it is not possible for providers to be in the same location, providers should still collaborate within a formal network of post-concussion care providers to allow for inter-professional communication, improved patient follow-up and increased efficiency of treatment. Telemedicine is an option in this case.
The pathway emphasizes that the patient should be seen by a healthcare professional for which it is within their scope of practice to provide a diagnosis of concussion and/or treatment based upon their professional competencies. The intention is that this pathway be a navigational tool through the current system of available care so that patients can receive appropriate, effective and timely care.
The Post-Concussion Pathway presented is a general overview to show how patients can navigate through appropriate post-concussion care, integrating both the public and private healthcare systems. It should be noted that there may be referrals to other healthcare practitioners to rule out concurrent diagnoses (i.e., medical specialists), and these other practitioners could also refer into this pathway to rule out the diagnosis of concussion. When there are co-existing, more physical injuries (for example, orthopedic injuries) some treatment can be initiated within the first few weeks without waiting the suggested time for determination of prolonged symptoms that require interdisciplinary care. In the interest of simplicity, all these possibilities are not included in the diagram. Evidence has been provided where possible to support the elements and the timing of care represented in the Pathway.
Key Messages
- The proposed pathway is grounded in evidence and is consistent with the best practice guidelines and established scopes of practice for different licensed healthcare professionals.
- Not everyone enters the pathway in the same way so it must allow for flexibility.
- Not everyone will need an interdisciplinary clinic, but there is still the need for all patients to get knowledgeable and appropriate care when needed.
- Persons whose symptoms have not resolved within 2 weeks should be re-assessed and considered for referral to an interdisciplinary clinic.
- There may be a need for referral to healthcare providers who are not directly involved in the Concussion Clinic. Referral indicators and risk factors have been identified.
Concussion Recovery Pattern
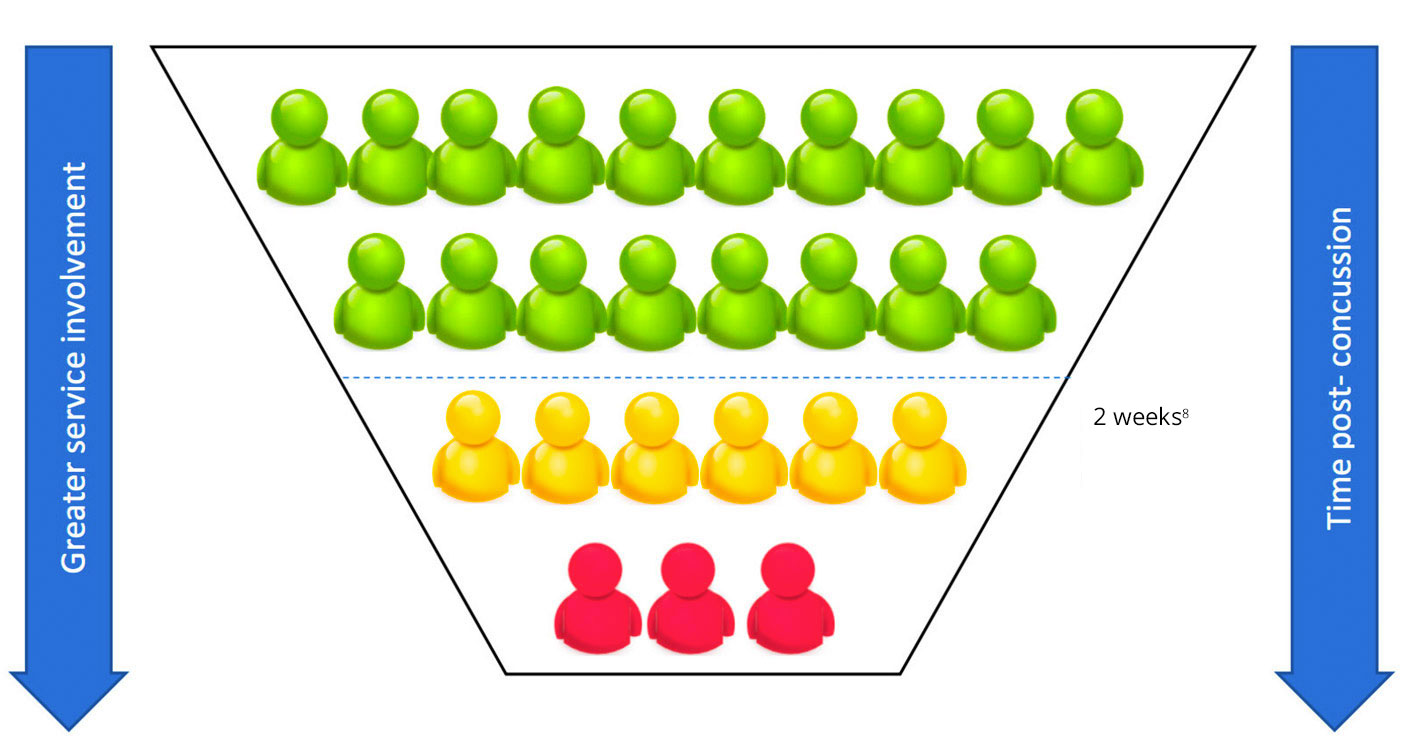
 Follow-up with primary care provider – majority will recover over a few days to weeks, with education about symptom management.
Follow-up with primary care provider – majority will recover over a few days to weeks, with education about symptom management.
 Follow-up required, further assessment may be required if symptoms are not resolving fully or considered as higher risk for a prolonged recovery.
Follow-up required, further assessment may be required if symptoms are not resolving fully or considered as higher risk for a prolonged recovery.
 Persistent symptoms, interdisciplinary care required.
Persistent symptoms, interdisciplinary care required.
Post-Concussion Care Pathway
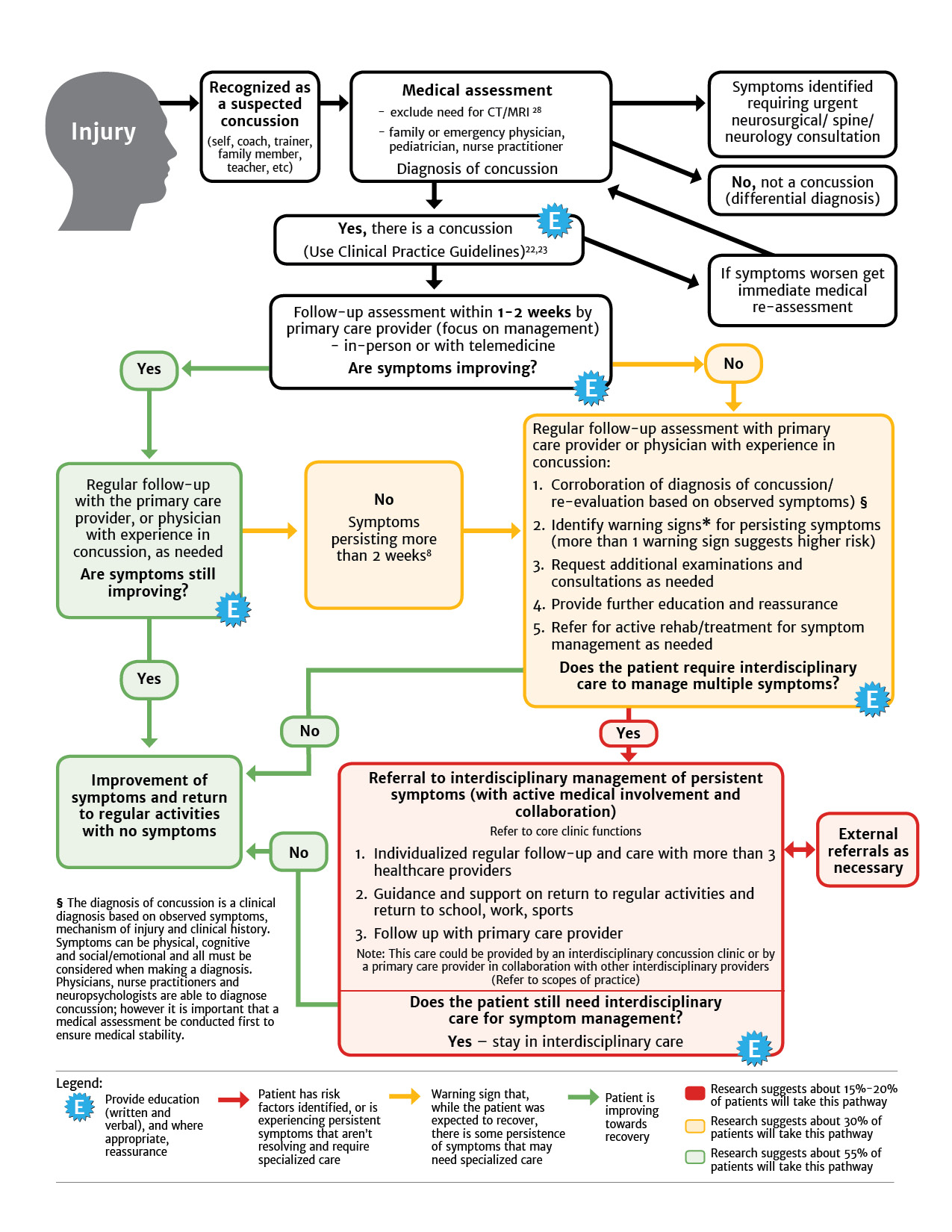
A patient can enter this pathway immediately, shortly following injury, or after a period of time when it is recognized that concussion-like symptoms are not resolving. It is necessary that all patients be properly assessed and diagnosed. Patients suspected of having had an earlier concussion should enter the pathway from the beginning so that they can be assessed and diagnosed by the appropriate professional.
* Warning Signs (risk factors) for poor prognosis
To learn more about the warning signs for poor prognosis, please see our resource: Pre-Injury or Acute Predictors of Prolonged Concussion Symptoms (> 1 Month Post-Injury) Based on Good Quality Studies.